Preventing Documentation Errors in Healthcare
Documentation errors in healthcare are far more than just minor typos or clerical mix-ups. They represent critical breakdowns in communication that can have devastating effects on patient lives.
We're talking about everything from wrong patient information and incorrect medication dosages to incomplete clinical notes. These aren't just administrative headaches; they introduce serious risks for both patients and the clinicians trying to care for them. At its core, the problem is that bad information leads to bad decisions, which can result in misdiagnoses, improper treatments, and significant legal fallout.
Why Documentation Errors Are So Dangerous

Think of a patient's medical record as the blueprint for their entire journey through the healthcare system. Just like an architect needs a flawless blueprint to build a stable structure, doctors and nurses rely on accurate, complete documentation to make sound decisions. A single incorrect measurement, a missing allergy note, or a mistyped lab result can throw the entire plan off course.
When that "blueprint" is flawed, the consequences can be catastrophic. These aren't just abstract what-ifs; they are real-world scenarios that play out in hospitals and clinics every single day. Many of the most severe patient safety events can be traced back to seemingly small documentation errors in healthcare.
The High Stakes of Inaccuracy
The real danger is how these mistakes completely disrupt the flow of critical information between members of a care team. A nurse might give the wrong medication because of an incorrect order. A surgeon could operate on the wrong site. A specialist might recommend a harmful treatment simply because a patient's full medical history wasn't available.
Here’s a look at what’s truly on the line:
- Patient Safety: This is the most immediate and serious concern. Errors can lead to life-threatening allergic reactions, delayed cancer diagnoses, or improper treatment plans that cause permanent harm, or worse.
- Clinical Decision-Making: Every diagnosis and treatment is built on the foundation of data in the medical record. If that data is wrong, the decisions will be wrong.
- Legal and Financial Liability: Inaccurate records are a massive driver of malpractice lawsuits. This can lead to crippling legal fees, steep regulatory fines, and lasting damage to a healthcare organization's reputation.
- Operational Integrity: Errors cause chaos. They require staff to spend valuable time hunting down correct information, lead to denied insurance claims, and disrupt the financial stability of a practice.
Accurate documentation is the bedrock of patient safety. When that foundation is shaky, the entire system of care becomes unstable, putting everyone involved at risk.
This guide will give you a full overview of this critical issue. We’ll explore the most common types of documentation errors, get to the bottom of their root causes, and lay out proven strategies for preventing them. Following the right protocols is key, and our Essential Guide to Healthcare Documentation Standards offers a much deeper dive into these requirements. To fully appreciate the seriousness of getting details right, it's also worth understanding the critical importance of labelling in healthcare, another area where precision is everything.
Mapping the Different Types of Documentation Errors
To really get a handle on preventing documentation errors, you have to know what you’re up against. These mistakes aren't a one-size-fits-all problem; they show up in different ways, and each one carries its own risks. It's like a domino effect—one small error in a patient's chart can set off a chain reaction that compromises their entire care plan.
A simple slip, like a misplaced decimal point in a lab result or a hastily jotted note, can spiral into a serious issue. That's why spotting the specific type of error is the crucial first move in creating a stronger, safer documentation process.
Omission vs. Commission: What's Missing vs. What's Wrong
At the most basic level, documentation errors fall into two major buckets: errors of omission and errors of commission. Think of them as two sides of the same coin.
- Errors of Omission (Missing Information): This is when critical information never makes it into the patient's record. Maybe a known drug allergy isn't noted, a complaint of chest pain isn't documented, or a sudden change in vital signs goes unrecorded. The real danger here is that the next clinician is making decisions with an incomplete puzzle.
- Errors of Commission (Incorrect Information): This happens when wrong information is actively recorded. It could be charting the wrong medication dosage, documenting a procedure on the wrong patient, or entering a lab value that is just plain wrong. These mistakes don't just create a gap—they actively send the care team down the wrong path.
An error of omission creates a blind spot. An error of commission creates a false trail. Both are incredibly dangerous.
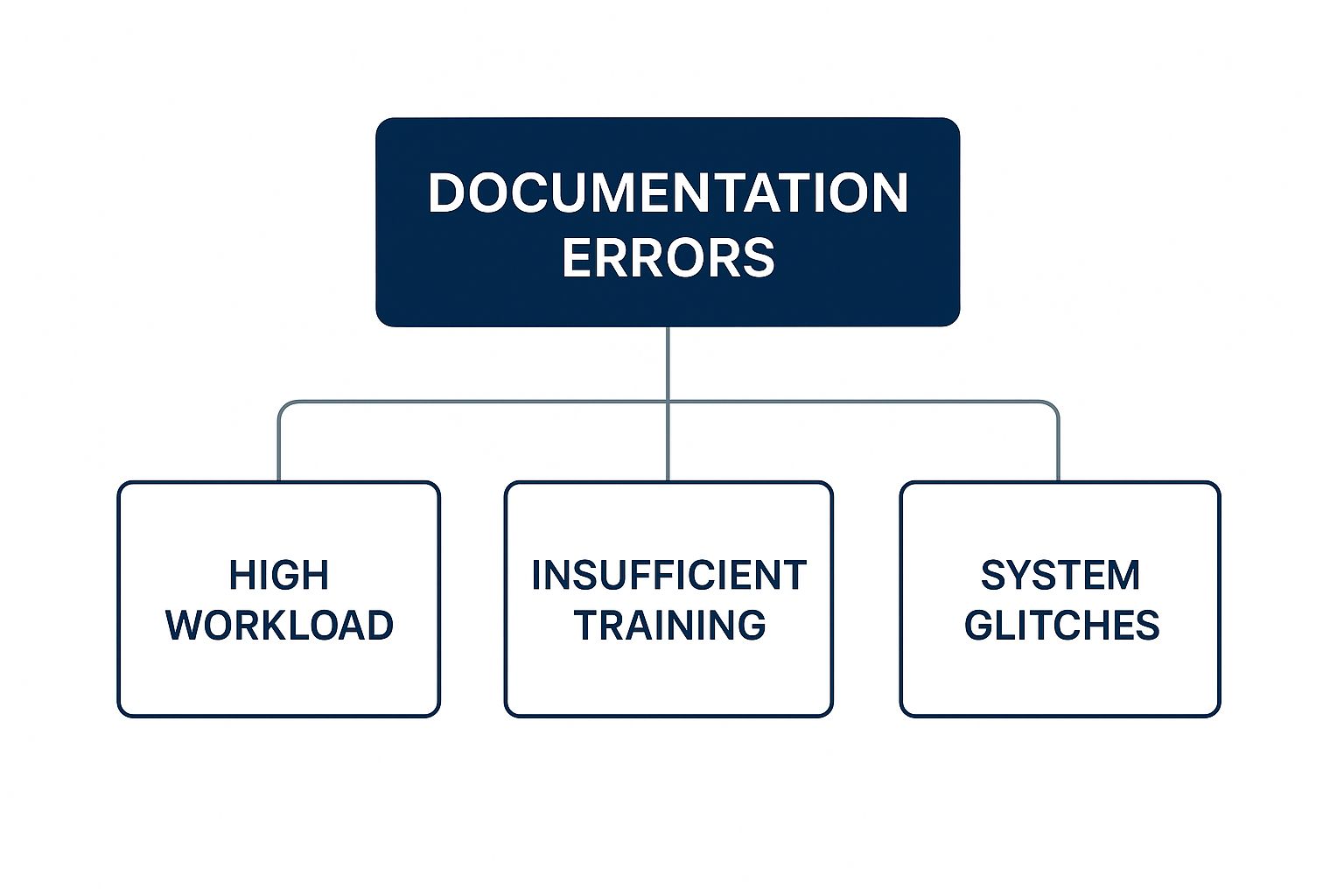
As you can see, factors like a high workload, insufficient training, and technology glitches create the perfect storm for these kinds of mistakes to happen.
To give you a clearer picture, here's a breakdown of common errors and the real-world impact they can have.
Common Types of Healthcare Documentation Errors and Their Potential Impact
| Error Type | Description & Example | Potential Clinical Impact |
|---|---|---|
| Omission | Failing to document a patient's known allergy to penicillin. | A physician, unaware of the allergy, prescribes an antibiotic in the penicillin family, leading to a severe allergic reaction. |
| Commission | Incorrectly charting a blood sugar reading of 180 mg/dL when it was actually 80 mg/dL. | The patient may be given insulin they don't need, causing a dangerous drop in blood sugar (hypoglycemia). |
| Sequencing | Documenting that a dose of pain medication was given before the patient reported severe pain. | This scrambles the clinical timeline, making it difficult to assess treatment effectiveness or understand the progression of symptoms. |
| Transcription | A verbal order for "fifteen milligrams" of a drug is misheard and transcribed as "fifty milligrams." | The patient receives a significant overdose, which could lead to toxicity or even be fatal depending on the medication. |
Each of these examples shows how a seemingly small clerical error can directly threaten patient safety.
Sequencing and Transcription Errors
It’s not just about whether the data is present or correct; the context and order are just as important. Two other common and critical errors highlight this perfectly.
Sequencing Errors: A patient’s medical record tells a story over time. A sequencing error jumbles up the timeline. For example, documenting that a medication was given before the order was even written, or charting that a symptom appeared after the treatment for it was administered. This twists the clinical narrative, which can easily lead to flawed diagnostic thinking and the wrong interventions.
Transcription Errors: These mistakes pop up whenever information is moved from one place to another. It happens all the time when transcribing spoken notes into text, copying lab results into an EHR, or moving data between systems. The classic example is mishearing "fifteen milligrams" as "fifty milligrams"—a simple slip of the ear with potentially fatal consequences.
Documentation errors are a major driver of medical mistakes around the world. They are tightly linked to diagnostic errors and are a direct cause of significant patient harm.
The numbers are truly sobering. Diagnostic mistakes, which frequently begin with bad documentation, are blamed for the death or permanent disability of 40,000 to 80,000 patients every year in the United States. What's more, an estimated 12 million patients in the U.S. experience a diagnostic error annually, and about a third of those cases result in harm. You can learn more about these findings on diagnostic errors and patient safety from the National Institutes of Health.
Getting familiar with these distinct types of errors is the first real step we can take to turn that tide and protect patients from preventable harm.
Getting to the Root of Inaccurate Documentation

To really fix documentation errors in healthcare, we have to look past the individual mistakes and dig into the environments where they grow. It’s almost never about one person being careless. More often, these errors are the predictable result of a perfect storm where system-wide pressures, human limits, and clunky technology all collide.
Understanding what causes these issues is the first real step toward building a stronger, safer system. Once we can pinpoint the why, we can stop just reacting to errors and start proactively preventing them. This means taking an honest look at all the interconnected reasons why accurate documentation is so tough in the whirlwind of a clinical setting.
The Weight of Systemic Pressures
Healthcare is a complex and often strained machine. This pressure-cooker environment can easily lead to documentation errors. Clinicians are working under immense stress, and sometimes the very systems meant to support them actually add to the problem.
Two big systemic culprits pop up again and again:
- High Patient Loads and Time Constraints: When a clinician is juggling a dozen or more patients in a single shift, time is the one thing they don't have. This forces them to rush through notes, often trying to recall details hours after seeing a patient. That's a recipe for leaving things out or getting them wrong.
- Inadequate Training and Standardization: A lack of clear, consistent documentation rules across a hospital or health system is a huge problem. What one department considers standard shorthand might be a source of complete confusion for another, creating dangerous communication gaps that can disrupt patient care.
These system-level issues basically set the stage for mistakes, making it incredibly difficult for even the most careful professional to keep every record perfect.
Human Factors and Cognitive Load
At the end of the day, clinicians are human. The sheer intensity of their work takes a toll. Fatigue, stress, and the brain's own shortcuts aren't character flaws; they're predictable results of working in such a high-stakes, high-pressure job.
Cognitive load—the amount of mental bandwidth a task requires—is a massive factor here. A doctor who is managing multiple complex cases, interpreting lab results, and talking with anxious families simply has less mental energy left for meticulous documentation.
Clinician burnout isn't just a wellness issue; it's a critical patient safety issue. A tired, overextended provider is far more likely to make a documentation error that could lead to real patient harm.
This is where our brains naturally try to take shortcuts. These mental shortcuts are great for making quick decisions, but they can backfire when it comes to documentation. A clinician might unconsciously fill in a gap with what they assume happened or copy information from a previous note that already had an error, keeping the mistake alive in the patient's record. If you want to dive deeper into this, you can explore strategies for improving clinical documentation from the inside out.
Technology Gaps and Usability Issues
Electronic Health Records (EHRs) were supposed to make everything better, but their rollout has created a whole new set of headaches. A poorly designed EHR can be more of a hindrance than a help, directly causing errors.
- Clunky User Interfaces (UI): Let's be honest—many EHRs just aren't easy to use. Clinicians often have to click through endless screens and dropdown menus just to enter one piece of information. This is what we call "click fatigue," and it makes it easy to put data in the wrong field or miss it entirely.
- Lack of Interoperability: When different systems can't talk to each other, you get dangerous information silos. If a patient's records from their family doctor can't be sent seamlessly to the hospital, critical details like allergies or current medications can get lost. This forces staff to re-enter information by hand, which opens the door to transcription errors.
It's also worth noting that our view of these problems is often skewed. A major analysis of over 5,700 publications found that a staggering 83.32% of all research on medical errors comes from high-income countries. This means the unique challenges faced in low- and middle-income regions—often related to limited resources and technology—are seriously under-studied.
By understanding how these three forces—systemic, human, and technological—all work together, healthcare organizations can start to dismantle the conditions that allow documentation errors in healthcare to happen. This is how we build a safer environment for everyone.
The Real-World Impact of Documentation Mistakes
It’s one thing to talk about the different types of documentation errors in healthcare, but it’s another to see the damage they cause firsthand. These aren't just abstract risks on a compliance checklist; they have real, sometimes devastating, consequences for patients and the very organizations meant to care for them.
The fallout from a single mistake can spread quickly, touching nearly every corner of the healthcare system. The impact can be split into two main areas: the direct clinical harm to patients and the severe legal and financial blowback for providers.
The Human Cost: Clinical Consequences
At its core, a documentation error is a breakdown in communication that puts patient safety on the line. The medical record is supposed to be the single source of truth for a patient's care. When that truth is wrong, clinicians end up making critical decisions based on faulty intelligence.
This can set off a chain reaction of preventable medical events. Think about these all-too-common situations:
- Misdiagnosis and Delayed Treatment: An incomplete patient history can send a physician down the wrong path. Forgetting to chart a persistent, low-grade fever could delay an infection diagnosis until it spirals into sepsis.
- Medication Mix-ups: A tiny transcription error, like putting a decimal in the wrong place, can turn a standard dose of medication into a toxic one. It's one of the most common and dangerous results of poor documentation.
- Surgical and Procedural Errors: Inaccurate records are a known contributor to wrong-site or even wrong-patient surgeries. If a pre-op checklist is based on a chart that’s already wrong, the whole safety protocol is compromised before the procedure even begins.
These clinical outcomes are where the true human cost lies. They transform routine care into high-stakes gambles and can leave patients with injuries that last a lifetime.
The Bottom Line: Legal and Financial Fallout
Beyond the immediate harm to the patient, the organizational fallout from documentation errors can be massive. Inaccurate or incomplete records are a leading cause of malpractice lawsuits, creating a huge legal and financial burden for healthcare providers.
In any legal battle, the patient's chart is the star witness. When that witness is full of inconsistencies, gaps, or outright mistakes, defending the quality of care becomes next to impossible.
The medical record is either your best defense or your worst enemy in a courtroom. An error-filled chart not only fails the patient clinically but also exposes the organization to significant legal and financial peril.
The damage doesn't end with a verdict. Healthcare organizations face a cascade of other serious consequences that hit their stability and public image hard.
Significant Organizational Risks
- Denied Insurance Claims: Payers comb through documentation to confirm that billed services were medically necessary and actually performed. Errors are a fast track to claim denials, leading to huge revenue losses. In fact, a recent report showed that 82% of denied claims are potentially avoidable with better documentation.
- Regulatory Fines and Penalties: Government agencies and accrediting bodies don't take documentation lightly. They can impose heavy fines for non-compliant or fraudulent records, with penalties that can run into the millions and cripple a budget.
- Reputation Damage: A major medical error or a big malpractice settlement can shatter a community's trust in its local hospital or clinic. Rebuilding that reputation can take years, if it can be done at all.
Ultimately, preventing these mistakes is about more than just checking boxes. It’s a core requirement for ensuring patient safety and keeping a healthcare organization healthy. For anyone looking to shore up their defenses, exploring effective clinical documentation improvement tips is the best place to start.
How Technology Can Help Reduce Documentation Errors
After digging into the causes and consequences of documentation mistakes, it's natural to start looking for a better way forward. While good old-fashioned human oversight and solid processes are non-negotiable, modern technology offers a powerful new line of defense against the constant threat of documentation errors in healthcare. The move from paper charts to the first wave of Electronic Health Records (EHRs) was just the start.
Now, we're seeing more advanced tools that act like a co-pilot for clinicians. They can catch potential errors as they happen and automate the tedious tasks that are often breeding grounds for mistakes. When put into practice thoughtfully, this technology doesn't replace a clinician's judgment—it supports it, creating a much safer and more efficient world for everyone involved.
The Rise of AI and Intelligent Automation
Artificial intelligence (AI) is no longer just a futuristic concept; it's becoming a practical part of everyday clinical workflows. AI-powered systems can scan massive amounts of unstructured data—things like clinical notes and dictated observations—to spot inconsistencies that a busy human might easily overlook.
Think of it this way: an AI tool could flag a contradiction where a doctor's note says a patient is a "non-smoker," but the patient's record also shows a prescription for a smoking cessation drug. That kind of intelligent double-check helps make sure the entire patient story adds up.
These systems are especially good at tackling some of the most common problems:
- Catching Inconsistencies: AI algorithms can cross-reference new entries against a patient's entire history, flagging conflicting diagnoses, allergies, or medication lists before they cause harm.
- Checking for Completeness: The software can gently nudge clinicians if a required field is empty or if a standard note template is missing key information, which helps cut down on errors of omission.
- Assisting with Coding: By analyzing clinical notes, AI can suggest the right billing codes. This takes a lot of guesswork out of the equation and reduces the manual coding errors that so often lead to denied claims.
Advanced Transcription and Speech-to-Text Solutions
One of the most common entry points for documentation errors is transcription—the simple act of turning spoken words into written text. Whether it's a doctor dictating notes or a nurse transcribing a verbal order, the risk of mishearing or mistyping is always there.
Technology designed to perfect the transcription process is a game-changer for documentation accuracy. By capturing spoken words with near-perfect precision, these tools virtually eliminate one of the most common pathways for critical errors to enter a patient's record.
This is where sophisticated solutions like Whisperit really shine. By using advanced AI models, these platforms capture dictation with incredible accuracy, which dramatically reduces the manual effort and error risk that comes with old-school transcription. You can learn more about how medical speech-to-text software is changing the game for healthcare providers.
The interface below shows just how much a clean, intuitive platform can simplify the work of documentation.
A streamlined design like this lets clinicians focus on what they're saying, not on battling a clunky system.
Let's compare the old way of doing things with this new, AI-assisted approach.
Comparing Manual vs AI-Assisted Documentation Methods
This table breaks down the key differences in accuracy, efficiency, and risk between traditional documentation practices and modern, AI-powered solutions.
| Feature | Manual Documentation | AI-Assisted Documentation (e.g., Whisperit) |
|---|---|---|
| Accuracy | Prone to human error (typos, misinterpretation) | High accuracy with AI-powered transcription and validation |
| Efficiency | Time-consuming, involves manual typing or dictation-review cycles | Near real-time transcription, freeing up clinician time |
| Error Detection | Relies on manual proofreading, often after the fact | Real-time flags for inconsistencies and missing information |
| Consistency | Varies by clinician and workload | Enforces standardized templates and terminology |
| Risk of Burnout | High administrative burden contributes to clinician burnout | Reduces administrative tasks, allowing focus on patient care |
As you can see, the move toward AI-assisted tools isn't just about speed; it's about building a fundamentally more reliable and less burdensome documentation process.
Breaking Down Silos with Interoperability
Even the best tools are only as good as the system they're in. Interoperability—the ability of different health IT systems to talk to each other and understand the data they share—is the glue that holds modern healthcare together. When systems can't communicate, you get data silos. That forces staff to manually re-enter information, opening the door for countless errors.
The scale of this data problem is staggering. Between 2020 and 2025, global healthcare data is expected to jump from 2,300 to 10,800 exabytes. And yet, as of 2021, only 46% of U.S. hospitals had achieved basic EHR interoperability. This disconnect is a huge source of waste, contributing to an estimated $30 billion in annual losses from redundant tests and other inefficiencies. You can dive deeper into this challenge and discover how AI is improving clinical data accuracy on estenda.com.
True interoperability ensures a patient’s complete, up-to-date record travels with them, whether they're visiting their primary care doctor, the emergency room, or a specialist. This seamless flow of information is absolutely critical for preventing dangerous medication errors, avoiding duplicate procedures, and giving every clinician the full picture they need to make the best decisions. By embracing these technological leaps, healthcare organizations can build a documentation ecosystem that is far more resilient and reliable.
A Practical Framework for Preventing Errors
Knowing what causes documentation errors is one thing; building a system to stop them is another. The key isn't a single magic bullet. It’s about creating a multi-layered defense built on three core pillars: People, Processes, and Technology.
When you reinforce each of these areas, you start to build a culture where accuracy becomes the default. It's how you shift from simply reacting to errors to proactively preventing them before they can cause harm.
Empowering Your People
Your first and most important line of defense against documentation errors in healthcare will always be your frontline clinicians. Giving them the right training and support is absolutely critical.
- Provide Continuous Training: Documentation standards are constantly changing. Don't just rely on a one-time onboarding session. Regular, engaging training keeps everyone up-to-date on best practices, new compliance rules, and how to use your systems effectively.
- Foster a No-Blame Culture: This is huge. Clinicians have to feel safe reporting errors or even near-misses without fearing punishment. When a mistake is treated as a learning opportunity for the whole system, you can uncover and fix the real root cause. This sense of psychological safety is the foundation of any truly reliable organization.
Refining Your Processes
Even the best people will stumble in a broken system. Strong, standardized processes are the guardrails that guide clinicians toward accurate documentation, especially when they're under pressure.
Start by creating standardized templates for your most common notes and procedures. This simple step ensures all the crucial information gets captured every single time, drastically reducing the risk of omissions. Regular chart audits are also essential—think of them as quality control checks. They help you spot recurring error patterns early so you can fix systemic problems before they get worse. Learning from technical documentation best practices outside of healthcare can also offer fresh insights to minimize common mistakes.
A strong process acts like a pilot's pre-flight checklist. It doesn't replace their skill or judgment, but it ensures critical steps are never missed, no matter how routine the flight may seem.
Leveraging the Right Technology
Finally, the right technology can be a powerful force multiplier. It can handle the tedious work and provide a smart safety net for your team.
- Choose User-Friendly Tools: Your EHR and other documentation software must have an intuitive interface. If a tool is clunky and frustrating, your staff will find workarounds, and those workarounds almost always bypass the built-in safety features.
- Integrate Smart Solutions: AI-powered transcription tools can all but eliminate dictation errors. Likewise, modern systems can have built-in alerts that flag potential inconsistencies or missing data in real-time, nudging the user to make a correction on the spot.
By weaving these three pillars together, you create a truly comprehensive defense against documentation errors.
Your Actionable Prevention Checklist
Turning these ideas into action is where the real work begins. Use this checklist to take stock of your organization’s practices and find areas to strengthen.
- People:
- Schedule quarterly documentation refresher courses.
- Establish a confidential, non-punitive error reporting system.
- Processes:
- Review and standardize your top five most-used documentation templates.
- Implement a monthly random chart audit protocol.
- Ensure your documentation protocols are legally sound. Our HIPAA compliance requirements checklist is a great place to start.
- Technology:
- Gather direct feedback from clinicians on EHR usability and pain points.
- Evaluate AI-driven tools that can automate transcription and flag potential errors.
Frequently Asked Questions
When you're dealing with the tangled web of healthcare documentation, a few key questions always seem to pop up. Let's tackle some of the most common ones to clear up the confusion around the legal, practical, and tech-related aspects of keeping patient records straight.
How Can You Legally Correct an Error in a Medical Record?
Fixing a mistake in a patient's chart isn't like hitting the backspace key. To keep the record legally sound, you can't just delete or white-out the original entry. The right way to do it is to draw a single, clean line through the incorrect information, making sure it's still readable.
Right next to it, add the correct information along with the date, time, and your initials. This approach creates a clear, honest audit trail that shows what was changed, when it was changed, and who changed it.
The golden rule for correcting a medical record is transparency. You're not trying to hide the mistake; you're amending it while preserving the original entry for full legal and clinical context.
What Is the Most Frequent Type of Documentation Error?
While there are many ways a chart can go wrong, errors of omission are incredibly common. This is when vital information simply never makes it into the record—a known allergy, a new symptom the patient mentioned, or a dose of medication that was given.
These omissions often happen when clinicians are swamped with high patient loads and feel rushed. In the hurry, details get missed. This creates dangerous blind spots that can seriously impact the next person providing care.
How Can Small Clinics Afford New Documentation Technology?
For smaller practices, the idea of investing in new technology can feel overwhelming, but it doesn't have to break the bank. Instead of a huge upfront cost, many clinics are turning to subscription-based models.
Software-as-a-Service (SaaS) platforms, like the new wave of AI transcription tools, offer affordable monthly plans. This gets rid of the need to buy expensive software licenses or manage complicated in-house servers. It gives smaller clinics access to the same powerful tools that reduce administrative work and boost accuracy, leveling the playing field.
Ready to eliminate transcription errors and reclaim valuable time? Whisperit provides an advanced AI dictation and editing platform that helps healthcare professionals create accurate, secure documentation up to two times faster. Discover the difference at https://whisperit.ai.