HIPAA Compliant Speech to Text a Practical Guide
The administrative burden in healthcare is a genuine crisis. Clinicians often find themselves spending just as much time on paperwork as they do with patients. This is why HIPAA-compliant speech to text has moved from a "nice-to-have" gadget to an essential tool for any practice that wants to reduce burnout while keeping patient privacy locked down. This technology is a direct route to getting precious time back without cutting corners on security.
Why Secure Speech to Text Is a Non-Negotiable
In any clinical environment, you're always fighting the clock. The constant need for efficiency runs head-on into the detailed, time-sucking reality of medical documentation. This isn't just an annoyance; it’s a major driver of physician burnout and can even affect patient care. When your team is drowning in paperwork, their focus is split, and energy is drained away from what actually matters: the person in the room.
This is precisely where the conversation about HIPAA-compliant speech to text needs to happen. We're not just talking about trading a keyboard for a microphone. It’s about completely rethinking a workflow that has become unsustainable for so many in the healthcare field. The aim is to build a system where accurate, detailed notes are captured as they happen, freeing up practitioners to be fully present with their patients.
The Real Price of Documentation Burnout
You’ve probably heard of "pajama time"—the hours doctors spend charting at home after a full day of seeing patients. It’s not a cute industry quirk; it points to a serious work-life balance problem. This administrative overload crushes morale, leads to high turnover, and ultimately makes the profession feel unsustainable.
The numbers don't lie. Physicians are now spending about 26.6% of their day on documentation, and then another 1.77 hours after work just to catch up. Older voice recognition software helped a bit, but modern AI-powered ambient scribes—built from the ground up for HIPAA compliance—are hitting accuracy rates as high as 98%. That kind of precision slashes editing time and directly attacks the administrative overload fueling the burnout crisis.
Getting a Handle on the HIPAA Security Rule
The Health Insurance Portability and Accountability Act (HIPAA) isn't a suggestion—it's federal law with hefty fines for violations. The Security Rule is the part that sets the standard for protecting any electronic protected health information (ePHI).
Here's a look at the official guidance straight from the Department of Health and Human Services (HHS):

This image gets to the heart of the Security Rule: you must ensure the confidentiality, integrity, and availability of all ePHI you create, receive, store, or send. Any speech-to-text tool you consider must have built-in safeguards to meet these exact requirements.
A common trap is thinking any encrypted service is automatically HIPAA compliant. It's not that simple. True compliance is a three-legged stool: it needs administrative, physical, and technical safeguards all working together to protect patient data from every angle.
Why Your Standard Transcription App Won't Cut It
Reaching for a generic, off-the-shelf transcription service for clinical notes is like walking a tightrope without a net. These tools simply aren't designed with the heavy-duty security needed for sensitive patient data. They're often missing crucial features like end-to-end encryption, granular access controls, or the audit trails needed to see who accessed data and when.
Even more importantly, most of these general-purpose vendors will never sign a Business Associate Agreement (BAA). Under HIPAA, a BAA is a legally binding contract that makes your vendor just as responsible for protecting PHI as you are. If you use a third-party service to handle patient data without a signed BAA, you are in direct violation of HIPAA. Simple as that.
For a closer look at the specific legal and technical boxes you need to tick, our comprehensive HIPAA compliance requirements checklist breaks it all down.
HIPAA Compliance in Speech to Text at a Glance
Navigating HIPAA can feel overwhelming, so I've put together this table to quickly summarize what truly matters when you're evaluating a speech-to-text service. These aren't just features; they are foundational requirements for protecting patient data and your practice.
| HIPAA Requirement | What It Means for Speech to Text | Why It's a Non-Negotiable |
|---|---|---|
| Business Associate Agreement (BAA) | The vendor must sign a BAA, legally obligating them to protect your PHI. | Without a BAA, you are in direct violation of HIPAA the moment PHI touches their servers. |
| End-to-End Encryption | Data is encrypted from the moment it leaves your device until it's stored, and back again. | Prevents unauthorized interception of sensitive patient conversations and notes. |
| Access Controls | Only authorized users can access specific patient data, based on their role. | Stops unauthorized employees or external parties from viewing sensitive information. |
| Audit Trails | The system logs every action taken on PHI (who, what, when). | Provides a crucial record for security reviews and breach investigations. |
| Data Disposal Policies | The vendor has a clear, secure process for permanently deleting PHI when required. | Ensures patient data isn't left lingering on servers indefinitely, reducing risk. |
Think of this table as your first-pass filter. If a potential vendor can't confidently check every one of these boxes, they aren't a serious contender for a healthcare environment.
Finding the Right HIPAA-Compliant Speech to Text Vendor

Choosing a HIPAA compliant speech to text provider isn't just another software purchase. It's a critical decision that puts your patients' most sensitive information—and your practice's legal standing—in the hands of a partner.
Get this right, and you’ll see a massive boost in efficiency. Get it wrong, and you're opening the door to serious compliance risks. This means you have to look past the slick marketing and really dig into what a vendor is offering, both technically and legally. It’s all about asking the right questions and knowing what a good answer looks like.
First Things First: The Business Associate Agreement
Let’s get the biggest deal-breaker out of the way immediately: the Business Associate Agreement (BAA). If a potential vendor can't or won't sign a BAA, walk away. Period.
This isn't optional. A BAA is a legally binding contract required by HIPAA that holds the vendor to the same high standards of PHI protection that you are. Without one, you're in immediate violation the moment any PHI touches their system. It’s the bedrock of a compliant partnership.
Make it a point to ask for their standard BAA early in your conversations. Then, have your legal counsel give it a thorough review.
A vendor’s hesitation to provide or discuss their BAA is a massive red flag. Any experienced, healthcare-focused company will have this process nailed down and will be completely transparent about their responsibilities.
Diving Deep into Security and Encryption
In the context of a HIPAA compliant speech to text service, true security is much more than a strong password. You need to confirm that the vendor has a robust, multi-layered security framework that protects data at every single point in its journey.
The conversation has to start with end-to-end encryption. This is non-negotiable. It means PHI is scrambled and unreadable from the moment a clinician speaks into a device, while it's being sent to the server for transcription (in transit), and while it’s being stored (at rest). Anything less creates vulnerabilities that can be exploited.
Beyond encryption, here are the security features you need to verify:
- Strict Access Controls: The system must let you define granular user permissions. This enforces the "minimum necessary" principle, ensuring staff can only access the specific patient data required for their jobs.
- Detailed Audit Trails: Every action involving PHI must be logged. You need to know who accessed data, what they did, and when. These logs are indispensable for security monitoring and are a core HIPAA requirement.
- Secure Data Centers: Ask where your data will live. Reputable vendors use high-security data centers that are compliant with standards like SOC 2 or ISO 27001.
The global speech-to-text API market, valued at USD 2.32 billion in 2021, is booming, largely driven by healthcare's needs. This surge underscores why you must prioritize security. You can discover more insights about the role of security in the speech-to-text market.
Is It Accurate? Does It Actually Work with Your EHR?
A tool can be locked down like Fort Knox, but if it’s wildly inaccurate or a pain to use, your team will simply find a way around it. High transcription accuracy is essential, especially when dealing with the unique lexicon of medicine.
A generic speech-to-text engine will trip over terms like "pharmacokinetics" or "sphygmomanometer." A solution built specifically for healthcare will be trained on medical language, improving its accuracy from day one. Always insist on a free trial or a pilot program to test the system with your own clinicians and their diverse accents and dictation styles.
Just as critical is seamless EHR integration. The speech-to-text service shouldn’t add another clumsy step to your documentation workflow. The best solutions plug directly into your Electronic Health Record (EHR), letting clinicians dictate straight into patient charts. This direct workflow eliminates the risky habit of copying and pasting PHI between different applications—a common cause of data leaks and costly errors.
Vendor Evaluation Checklist Key Features
When you're comparing different speech-to-text vendors, it’s easy to get lost in the details. This checklist breaks down the most critical features to look for, helping you make a direct, apples-to-apples comparison and spot potential issues before you commit.
| Feature | What to Look For | Red Flags to Watch For |
|---|---|---|
| HIPAA Compliance | Willingness to sign a Business Associate Agreement (BAA) without hesitation. Clear documentation of their compliance measures. | Hesitation or refusal to sign a BAA. Vague answers about their security protocols. |
| Encryption | End-to-end encryption is explicitly stated. Data is encrypted both in transit and at rest using strong algorithms (e.g., AES-256). | Mentions of "secure servers" without specifics on encryption. Encryption that only covers data at rest, but not in transit. |
| Access Controls | Role-based access controls (RBAC) that let you define granular permissions for different user types (e.g., clinician vs. admin). | A "one-size-fits-all" user permission model. Inability to restrict access based on job function. |
| Audit Trails | Comprehensive, immutable logs of all user activity involving PHI. Logs should be easily accessible for audits. | No audit trail functionality or logs that can be edited or deleted by users. |
| Transcription Accuracy | A specialized medical vocabulary. AI models trained on clinical data. High accuracy rates demonstrated during a pilot or trial period. | Generic, consumer-grade speech recognition engine. Poor performance with medical terminology or diverse accents during testing. |
| EHR Integration | Direct, API-based integration with your specific EHR system. A seamless workflow that doesn't require copy-pasting. | Clunky, non-native integrations. Requiring manual data transfer between applications, which introduces risk. |
Using a structured checklist like this ensures you don't overlook a crucial component. The right partner will be able to confidently check every one of these boxes, giving you peace of mind that your data is not only secure but that the tool will genuinely improve your clinical workflows.
Your Implementation and Rollout Roadmap
Successfully bringing a HIPAA compliant speech to text solution into your practice isn't something that happens overnight. You can't just flip a switch. It’s a deliberate process that, when planned thoughtfully, can be rolled out without disrupting the daily rhythm of your practice. A solid roadmap is what ensures the technology isn't just installed, but actually used and embraced by your team.
The first step is taking an honest look at your current workflows. Before you can fix the bottlenecks, you have to know exactly where they are. This means getting out there and talking to your clinicians and administrative staff to understand their biggest documentation headaches.
Start with a Realistic Needs Analysis
Don't just assume you know what everyone needs. A surgeon's dictation requirements are a world away from those of a physical therapist or a primary care physician. You need to sit down with these different groups and ask the right questions.
- Where is the most time actually lost? Is it during the initial note-taking, the tedious process of editing transcriptions, or the clumsy transfer of text into the EHR?
- What are the biggest accuracy challenges? I've seen certain medical specialties with unique terminology struggle way more than others. Find out who they are.
- Which workflows are the most rigid? Pinpoint the processes where a change could cause the most friction. That's where you'll need to plan for extra support and training.
Getting answers to these questions gives you a crystal-clear picture of what your practice actually needs. This insight is gold; it’s what helps you choose a solution that solves real, tangible problems instead of just adding another layer of tech for people to learn.
Vetting Vendors and Planning a Pilot Program
Once you know what you need, you can start talking to vendors with a specific checklist in hand. Beyond just ticking the security boxes, your focus should be on verifying their claims. Always ask for their security documentation, but here's the real test: ask if they will sign a Business Associate Agreement (BAA).
If a vendor even hesitates on the BAA, walk away. They are not a viable option for any healthcare provider, period.
A small-scale pilot program is your best friend during this phase. Instead of a high-risk, practice-wide launch, pick a small, tech-savvy group of users from different departments. This creates a safe, controlled environment to see how the software performs in the real world. The whole point of the pilot is to get honest feedback and spot potential issues before they impact everyone.
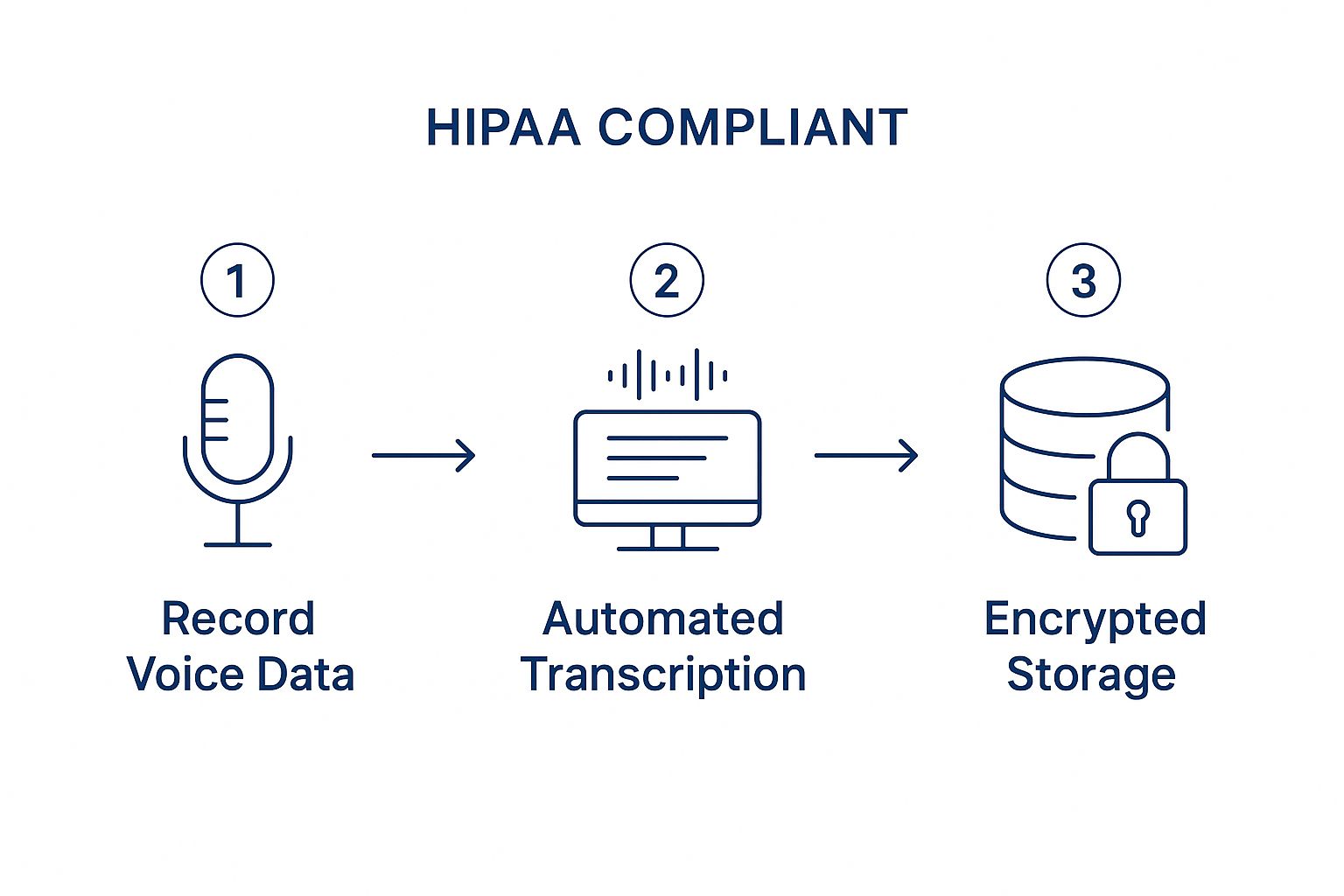
Think of it like a dress rehearsal. It’s your chance to work out the kinks, build confidence among a core group of users, and gather those crucial testimonials that will help win over skeptical team members down the line. As the graphic shows, it all boils down to a secure process: secure recording, automated transcription, and encrypted storage. That's the backbone of any system you can trust.
Configuration and a Phased Rollout
With a successful pilot under your belt, you’re ready to configure the system for a wider audience. This is where you can really make the software feel like it was tailor-made for your practice.
Some of the most impactful configuration steps include:
- Creating Custom Vocabularies: This is a game-changer. Add your practice-specific terms, physician names, and common local acronyms to the software's dictionary. This one step can dramatically boost transcription accuracy right out of the gate.
- Setting Up User Permissions: Implement role-based access. This ensures clinicians and staff can only access the information necessary for their jobs, keeping you in line with the "minimum necessary" principle required by HIPAA.
- Building Document Templates: Pre-load your common report formats, like SOAP notes or referral letters. This helps speed up the documentation process even more and is a key part of building an effective healthcare document management system that your team will actually appreciate.
Finally, resist the temptation to launch for everyone at once. A phased rollout is always more effective and far less disruptive. Start with the departments or teams that were most enthusiastic during the pilot. Their success stories will build momentum, making every subsequent rollout much smoother and fostering a culture of adoption, not resistance.
Getting Your Team On Board and Trained for Success
Choosing a great, HIPAA compliant speech to text solution is a huge step, but it’s only half the journey. A brilliant piece of tech is just a shiny new icon on the desktop if your team doesn't embrace it. The human side of adopting new technology is always the trickiest part, but with a smart approach, you can turn potential friction into genuine enthusiasm.
The secret is to make this transition feel like a genuine upgrade, not just another administrative burden. Your training needs to focus on real-world benefits that matter to your clinical and admin staff. It’s all about showing them how this tool gives them back precious time, rather than just adding another task to their already packed day.
Creating a Culture of Buy-In
Before you even think about scheduling the first training session, you have to answer the unspoken question on everyone's mind: "What's in it for me?" Let's be honest, your team is busy, and change can feel like a disruption. You need a compelling reason for them to get on board.
Instead of a generic memo, frame the rollout around solving the specific frustrations you’ve already identified. Talk about how it will slash "pajama time"—those extra hours clinicians spend catching up on notes at home. When your team sees a direct line between this new tool and a better work-life balance, adoption feels less like a mandate and more like a lifeline.
The best adoption strategies don't just teach clicks and features; they connect the technology directly to a better quality of life for the user. Show them a path to leaving work on time, and you'll have their full attention.
How to Design Training That Actually Sticks
Ditch the idea of long, mind-numbing lectures in a conference room. Effective training for a HIPAA compliant speech to text tool has to be short, practical, and tailored to specific roles. Your team doesn’t need a manual on every single feature; they need to know how to do their core tasks faster.
Here’s what I’ve seen work time and again:
- Train Workflows, Not Just Features: Don't just show off the software. Guide them through a complete, realistic task. For example, walk through dictating a full SOAP note directly into a patient’s chart in your EHR.
- Arm Them with Quick-Reference Guides: Create simple, one-page PDFs or laminated cards with the most common commands and simple troubleshooting tips. It's an easy-to-grab resource that won't interrupt their flow.
- Empower "Super-Users": Pick a few tech-savvy and respected people from different departments to be your internal champions. Give them some extra training and let them be the first line of support for their peers—it's often much less intimidating than calling IT.
Focusing on these practical, hands-on elements makes the training feel immediately relevant and useful. As part of this education, giving your team context on the different types of medical speech to text software available can help them appreciate the solution you've chosen.
Tackling Resistance and Celebrating Progress
Even with the best plan, you’ll probably run into some skepticism. That's normal. Some team members might worry about transcription accuracy or feel that talking is slower than their typing.
The best way to address this is with proof and peer influence. Share hard numbers from your pilot program, like the average time saved on documentation per patient. Even better, have your newly minted "super-users" share their own positive experiences at a staff meeting. A testimonial from a trusted colleague is worth more than any directive from management.
Finally, make a point to celebrate the wins, no matter how small. When a department gets fully up and running on the new workflow, give them a shout-out. This kind of positive reinforcement creates momentum and shows any holdouts that it’s time to get on board. Before you know it, the tool will go from being a "new requirement" to an essential part of how you work.
Keeping Your System Compliant and Optimized for the Long Haul

Getting a HIPAA compliant speech to text solution up and running is a huge step, but it’s not a one-and-done project. True compliance isn't something you can set and forget. It's an ongoing commitment—a continuous process of monitoring and refining that protects your patients and your practice long after the initial rollout.
Think of it less like installing a piece of software and more like adopting a new, fundamental standard of care for your data. This is where many practices stumble; they assume the technology handles everything. But to maintain compliance and really get your money's worth, you need a proactive strategy for the long term.
Make Security Reviews a Routine
The world of digital threats is always changing, so your security measures have to keep up. You can't just rely on the promises your vendor made during the sales pitch. One of the most critical habits to build is scheduling regular, recurring security reviews of your speech-to-text system.
This isn't as intimidating as it sounds. Your routine should cover a few key areas:
- Check the Access Logs: Get in the habit of reviewing audit trails for any red flags. Are you seeing logins at 3 a.m. or a series of failed access attempts from a single user? That could signal a compromised account.
- Audit User Permissions: At least quarterly, go through your user accounts. Make sure access levels still follow the "minimum necessary" rule. If someone’s role has changed or they’ve left the practice, their permissions need to be updated or removed immediately.
- Install Updates Promptly: Keep an eye out for emails from your vendor about security patches or software updates. Applying these right away is one of the easiest and most effective ways to close newly discovered vulnerabilities.
This kind of consistent oversight turns compliance from a passive checklist item into an active, defensible part of your operations. It’s how you ensure your handling of PHI stays secure over time. These principles apply to more than just dictation, as detailed in our guide on HIPAA compliant document sharing.
HIPAA compliance is a living process, not a destination. Regular security audits and active monitoring are the only ways to ensure your practice remains protected against evolving threats and avoids costly compliance gaps.
Fine-Tuning for Peak Performance
Security is non-negotiable, but don't forget about performance. Continuous optimization is what keeps your speech-to-text tool a valuable asset that your team actually wants to use. A system that’s slow, inaccurate, or clunky will just drive everyone back to their old, inefficient habits.
So, listen to your users. They are your single best source of feedback. If a clinician complains that the system always butchers a specific medication name, that’s your cue to investigate.
Create a simple feedback loop—a shared document, a dedicated email, whatever works—for your team to report issues or suggest improvements. You can use this input to refine the system. For example, by analyzing how the tool is used, you might find that certain documentation workflows are still hitting roadblocks. That data could point you toward creating a new template or tweaking the custom vocabulary, making the tool faster and more accurate for everyone.
Real-World Impact: The Ripple Effect Beyond Just Transcription
Theory is one thing, but seeing a HIPAA-compliant speech-to-text solution in action is where you grasp its true value. Yes, its core job is to turn spoken words into text, but that simple function creates a powerful ripple effect, touching every part of a clinical workflow. These aren't just abstract ideas on a feature list; they are real, measurable improvements you’ll see day in and day out.
Picture a busy speech therapist wrapping up her last session. Instead of staring down two hours of charting, she pulls up a template on her tablet, dictates her SOAP notes in a few minutes, and has the report signed and filed before she even walks out the door. This isn't some futuristic dream—it's what’s happening right now when smart, secure technology meets the real demands of a modern healthcare practice.
Redefining What Clinical Efficiency Looks Like
The first thing everyone notices is the massive drop in documentation time. For so many clinicians, charting is the biggest administrative headache—a constant grind that bleeds into personal time and is a major driver of burnout. When you slash the time they spend hunched over a keyboard, you’re not just speeding up a task. You're fundamentally improving their quality of life.
Take a multi-physician clinic struggling to keep up with patient flow. By bringing in a solid speech-to-text tool, they can cut the time it takes to write a patient note from a draining 15 minutes down to just five. That reclaimed time is huge. It means they can see more patients, slash wait times, and boost staff morale as that looming backlog of charts finally starts to shrink.
This shift is especially profound in specialized fields like speech therapy. The data shows a remarkable transformation: this technology can reduce documentation time by up to 70%. That efficiency boost means more time for actual patient care, which in turn leads to a 60% reduction in documentation errors. We've also seen same-day discharge summary completion jump from a mere 40% to an incredible 95%. As the administrative burden lightens, therapist satisfaction has been shown to climb by 35%, with compliance audit scores improving from 78% to 96%.
A Big Leap in Accuracy and Compliance
Let’s be honest: human error is a given with manual data entry, especially at the end of a long, stressful shift. A tired clinician is far more likely to make a typo or forget a key detail when typing notes from memory. A high-quality speech-to-text system, one that's been trained on medical terminology, acts as a crucial safety net.
The system captures the clinician’s exact words, creating a precise, verbatim record of the encounter. This doesn't just lower the risk of clinical mistakes caused by bad documentation; it also makes your compliance posture rock-solid. Armed with detailed, time-stamped, and accurately transcribed records, your practice is infinitely better prepared for an audit or quality review.
The real win here is creating a single, reliable source of truth for every patient interaction. When you capture documentation accurately at the point of care, you eliminate the dangerous game of trying to recall details hours later. The result is a safer, more defensible clinical record.
Improving the quality and timeliness of notes is a cornerstone of effective care. For a deeper dive into this subject, check out our guide on improving clinical documentation.
Measurable Wins for Your Practice
These benefits aren't just feel-good stories; they show up clearly in your operational metrics. When practices adopt a HIPAA-compliant speech-to-text solution, they see tangible progress in a few key areas:
- Faster Report Turnaround: What once took days can now be done in hours, if not minutes. This directly speeds up billing cycles and makes communication with referring physicians much smoother.
- Lower Transcription Costs: If you're still paying for external transcription services, bringing this process in-house with an automated tool can deliver some serious cost savings right to your bottom line.
- Better Staff Retention: People notice when you invest in tools that reduce their administrative burden and fight burnout. A happier, less-stressed team is a team that sticks around for the long haul.
Ultimately, all these benefits feed into a positive cycle. Clinicians feel more empowered and less overwhelmed, which leads to better patient care. The practice runs more efficiently, which strengthens its financial health. This technology isn't just about typing less—it's about building a more sustainable and effective healthcare environment for everyone involved.
Got Questions? We've Got Answers
Diving into the world of HIPAA-compliant speech-to-text can feel like navigating a minefield. It's totally normal to have questions. Let's clear up some of the most common ones that come up when healthcare professionals start exploring this technology.
Can a Cloud-Based Speech-to-Text Tool Actually Be HIPAA Compliant?
Yes, it absolutely can be, but you have to be careful. The key is that the cloud vendor can't just be any off-the-shelf service; they must be specifically set up to handle sensitive healthcare data. This isn't a "maybe"—the rules are black and white.
A compliant cloud partner must, without exception, sign a Business Associate Agreement (BAA). This is a non-negotiable legal contract that makes them just as responsible for protecting data as you are. They also need to provide things like end-to-end encryption and strict access controls. Grabbing a generic cloud transcription tool that doesn't offer these specific protections is a definite compliance violation.
What's the Big Deal with a Business Associate Agreement (BAA)?
Think of a Business Associate Agreement, or BAA, as the legal foundation of your relationship with any third-party vendor who might come into contact with Protected Health Information (PHI). It's a formal contract that lays out exactly how that vendor will protect the patient data you entrust to them.
A BAA is your legal safeguard. It contractually obligates your tech partner to uphold the same rigorous patient data security standards you do. If a vendor is unwilling to sign one, walk away. It's a massive red flag.
This document gets into the nitty-gritty: the specific security protocols they must use, what happens if there’s a data breach, and how they’re allowed to use PHI. The second your patient data hits their system without a signed BAA in place, you’ve fallen out of compliance.
How Accurate Is Medical Speech-to-Text, Really?
Honestly, the accuracy of today's medical speech-to-text tools is pretty incredible, but it's not all created equal. The top-tier solutions, the ones built specifically for medicine, can hit accuracy rates of 98% or even higher. They're designed to handle the tough stuff—complex medical jargon, thick accents, and even doctors who talk a mile a minute.
These systems are so good because their AI models have been trained on millions of hours of real clinical dictations. This means they understand the difference between "hypotension" and "hypertension," something a standard consumer app would likely miss. Many of these platforms also get smarter over time, learning your unique speech patterns and the specific corrections you make.
My best advice? Always run a trial or pilot program first. Let your own team put the software through its paces in their daily workflow. It's the only way to know for sure if its accuracy is good enough for your practice before you make a bigger commitment.
Ready to reclaim your time from clinical documentation? Whisperit offers a secure, AI-powered dictation platform designed for the privacy and accuracy demands of healthcare professionals. Reduce your paperwork by up to 2x and focus on what matters most—your patients. Discover how at https://whisperit.ai.