A Guide to Healthcare Quality Improvement Initiatives
Imagine a high-performance racing pit crew. Every single movement is measured, analyzed, and fine-tuned to shave off precious milliseconds and, most importantly, keep the driver safe. Healthcare quality improvement initiatives bring that same obsessive, data-driven focus to patient care. It’s about moving beyond just ticking boxes to proactively making things better for patients and staff.
Unpacking Healthcare Quality Improvement Initiatives

At their heart, these initiatives are structured projects designed to solve real-world problems in healthcare. We're not talking about vague goals like "improve patient happiness." Instead, we're targeting specific, measurable issues—like cutting down ER wait times, reducing hospital-acquired infections, or making sure every patient gets the right medication at the right time.
This systematic approach is what separates good healthcare systems from great ones. It's about building a culture where everyone, from the front desk to the operating room, feels empowered to ask, "How can we do this better?"
The Core Dimensions of Quality
So, what exactly are we trying to improve? Healthcare quality isn't just one thing. It's usually broken down into several key areas, which gives improvement teams a clear target to aim for.
- Safety: First and foremost, do no harm. This means preventing errors, accidents, and injuries that can happen during care. A huge part of this is focusing on solid strategies for healthcare-associated infection prevention.
- Effectiveness: Are we providing care that's backed by solid science? This is about ensuring patients get treatments that are proven to work and avoiding those that aren't.
- Patient-Centeredness: The patient is the expert on their own life. This dimension focuses on providing care that respects individual preferences, needs, and values.
- Timeliness: Waits and delays aren't just frustrating; they can be harmful. Timeliness means getting patients the care they need, right when they need it.
- Efficiency: This is all about avoiding waste—whether that's wasted supplies, wasted time, or wasted energy. More efficiency means more resources for direct patient care.
- Equity: Everyone deserves high-quality care, regardless of their gender, race, income, or where they live. Equity means closing the gaps in care quality for all populations.
Why These Initiatives Are Not Optional
This isn't just about striving for excellence; it's a matter of life and death. In low- and middle-income countries, a staggering 5.7 to 8.4 million deaths each year are due to poor-quality care. That accounts for up to 15% of all deaths in those regions, highlighting the urgent, global need for these programs.
A successful healthcare quality improvement initiative is a continuous cycle, not a one-time fix. It involves identifying a problem, implementing a change, measuring the results, and then refining the approach based on that data.
This constant feedback loop is the engine of improvement. Every touchpoint in a patient's journey, from the moment they walk in the door to the day they go home, is an opportunity for refinement. You can dig deeper into this process in our guide on https://www.whisperit.ai/blog/healthcare-process-improvement, which shows how even small tweaks can lead to major wins for patients and providers.
Choosing the Right Quality Improvement Framework
Just as a master carpenter has more than just a hammer in their toolbox, a healthcare leader needs the right tool for the right problem. Healthcare quality improvement initiatives aren't a one-size-fits-all game. They depend on structured frameworks—proven blueprints that guide teams from identifying an issue to creating a lasting solution. Picking the right one is your first, and most critical, step toward making a real difference.
Think of these frameworks as different recipes for success. Some are for quick, simple fixes, while others are built for complex, system-wide changes where every detail matters. Understanding the philosophy behind each one helps you match the method to the madness, ensuring your efforts are focused and effective.
The PDSA Cycle: Simplicity in Action
The Plan-Do-Study-Act (PDSA) cycle is the Swiss Army knife of quality improvement. It's straightforward, versatile, and incredibly powerful for testing changes on a small scale before you commit to a major overhaul.
Imagine a clinic where patients are frustrated with long wait times. Instead of redesigning the entire scheduling system overnight, the team could use PDSA to test one small tweak.
- Plan: The team has a hunch: what if sending paperwork to patients electronically before their visit could cut check-in time by five minutes? They decide to test this with 10 patients on a Tuesday.
- Do: On test day, they send the forms and carefully track the check-in times for those 10 patients.
- Study: Now, they look at the data. Did it work? Were there any tech glitches? What did patients and staff think about the new process?
- Act: Based on what they learned, they might decide to simplify the online form and run another small test. This is the essence of another PDSA cycle.
This iterative approach keeps risk low and allows for fast, continuous learning. It's perfect for teams that need to build momentum with small, tangible wins.
Lean Methodology: Eliminating Waste
Originally from the hyper-efficient world of manufacturing, Lean methodology is laser-focused on one thing: maximizing value by getting rid of waste. In healthcare, "waste" is much more than just expired supplies; it's anything that doesn't directly contribute to better patient care.
Common examples of waste you’d find in any hospital or clinic include:
- Waiting: Patients waiting for a doctor, or nurses waiting for lab results.
- Overproduction: Running unnecessary tests "just in case."
- Transportation: Moving a patient from one end of the hospital to the other for a simple scan.
- Defects: Medical errors, hospital-acquired infections, or misdiagnoses.
By mapping out a process—like a blood sample's journey from a patient's arm to the lab—a Lean team can easily spot bottlenecks and pointless steps. The goal is to create a smoother, more direct workflow that helps both patients and providers. For a broader perspective on this, our guide on various business process improvement methods offers some great insights.
Six Sigma: Pursuing Perfection
If Lean is about speed and efficiency, Six Sigma is about being as close to perfect as humanly possible. This is a highly disciplined, data-heavy framework designed to stamp out defects and variability in critical processes. The name itself comes from a statistical goal: limiting errors to just 3.4 per million opportunities.
Six Sigma is best reserved for high-risk, complex problems where the cost of error is extremely high—such as medication administration, surgical procedures, or diagnostic accuracy. It's the heavyweight champion of quality improvement frameworks.
It operates on a structured five-phase approach known as DMAIC:
- Define: Pinpoint the exact problem, the project goals, and what patients need.
- Measure: Gather data to establish a baseline of how the process is currently performing.
- Analyze: Dig into the data to find the true root causes of the problem.
- Improve: Develop, test, and roll out solutions that address those root causes.
- Control: Put systems in place to make sure the improvements stick.
This rigorous method requires a solid grasp of statistics, but it can produce dramatic, life-saving improvements in safety and reliability.
Before we move on, let's put these frameworks side-by-side to see how they stack up.
Comparing Quality Improvement Frameworks
| Framework | Core Principle | Best For | Example Application |
|---|---|---|---|
| PDSA Cycle | Iterative, small-scale testing | Rapid, incremental changes and testing new ideas with minimal risk | Testing a new patient check-in script to improve satisfaction scores. |
| Lean | Eliminate waste, maximize value | Improving process flow, reducing delays, and increasing efficiency | Redesigning a pharmacy's workflow to reduce medication dispensing time. |
| Six Sigma | Reduce defects and process variation | High-risk, complex problems where precision and safety are critical | Decreasing the rate of surgical site infections to near-zero. |
Ultimately, choosing the right framework depends entirely on the problem you're trying to solve. Each offers a unique path to a common goal: better, safer, and more efficient patient care.
The image below shows some of the core metrics used to assess the impact of these improvement initiatives.
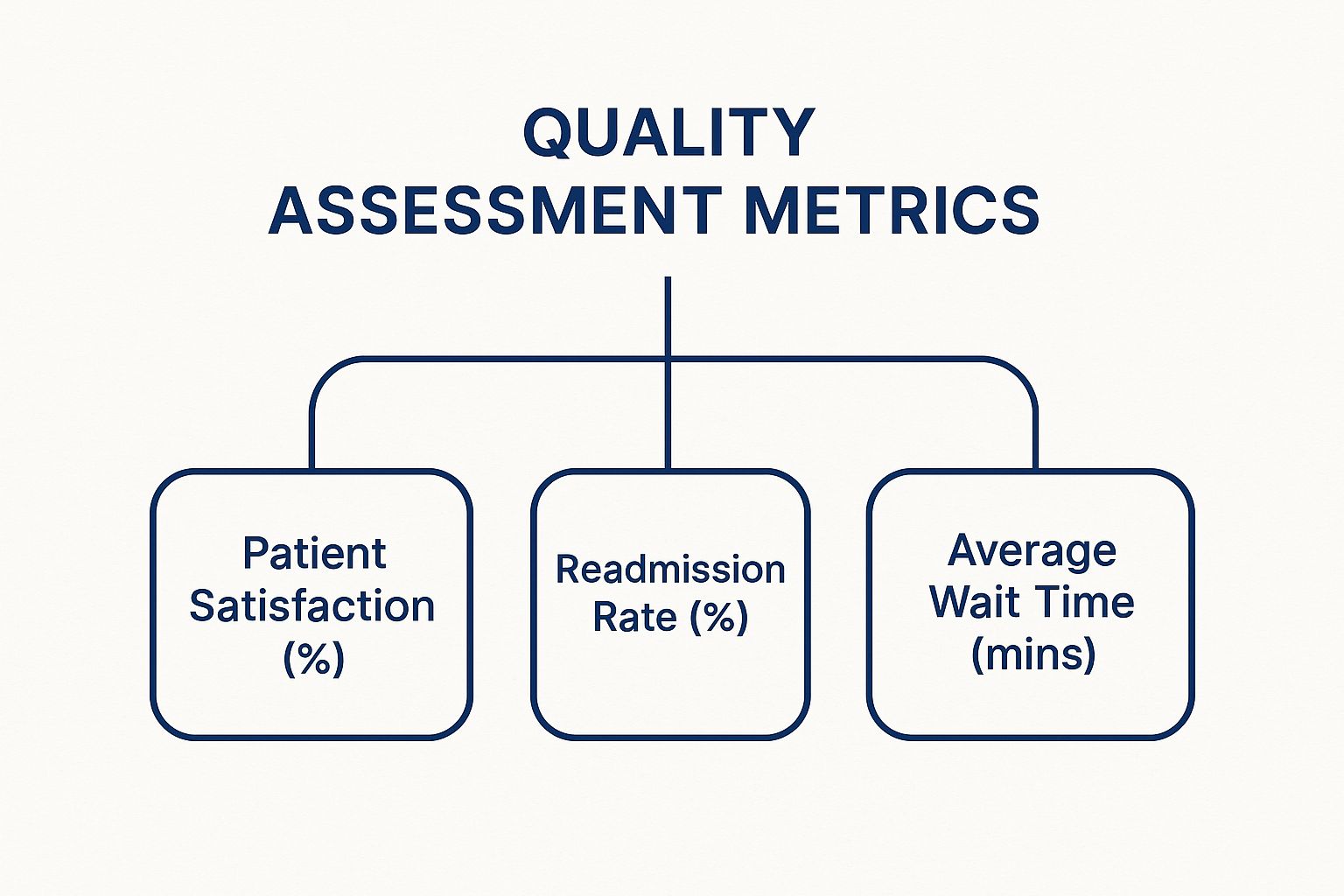
As you can see, these frameworks are designed to directly target key performance indicators like patient satisfaction, readmission rates, and wait times, turning abstract goals into tangible results.
How Do You Know If Your Initiatives Are Actually Working?

You’ve heard it a million times: you can't improve what you don't measure. In healthcare, this isn't just a business cliché—it's a fundamental truth. For any healthcare quality improvement initiative to be worth the effort, you need a scoreboard. This isn’t about collecting data to fill binders; it’s about using real numbers as a compass to guide your decisions and prove your changes are truly helping patients.
Moving beyond a vague feeling that "things seem better" means getting specific with what you track. The right metrics turn your quality goals into tangible, visible results, showing your team exactly where you're winning and where you might need to rethink your approach.
Choosing Your Core Metrics
The trick is to pick a balanced set of measures that paint a complete picture. Focusing on a single number can be incredibly misleading. Instead, experienced teams track three distinct types of metrics to get the full story.
- Process Measures: These check if you're actually doing the things you set out to do. They answer the question, "Are we following the new plan consistently?"
- Outcome Measures: This is the bottom line. These metrics track the direct impact on patient health and well-being. They answer, "Are our actions improving patient care?"
- Balancing Measures: Every change has the potential for unintended side effects. These metrics keep an eye on other parts of the system to make sure your improvements in one area aren't accidentally causing new problems somewhere else.
Let’s say a hospital wants to reduce patient falls. The team decides to implement a new risk assessment protocol that nurses must perform at the start of every shift.
A strong measurement strategy acts like a GPS for your project. Process measures tell you if you're following the route, outcome measures confirm you're getting closer to your destination, and balancing measures warn you about unexpected traffic jams or detours.
In this scenario, a key process measure would be the percentage of patients who receive the fall risk assessment within one hour of a shift change. The main outcome measure is obvious: the number of patient falls per 1,000 patient-days.
But what about a balancing measure? A good one might be nurse satisfaction scores. This helps ensure the new protocol isn't creating an overwhelming workload or causing burnout, which could lead to other issues. You can explore more ideas in our guide to quality assurance metrics examples.
Turning Data Into Clear Insights
Raw numbers in a spreadsheet can make your eyes glaze over. This is where data visualization comes in, turning columns of figures into a clear story about your progress. Good visuals help you spot meaningful trends and ignore the random noise.
Two of the most valuable tools for this are run charts and control charts.
Run charts are simple line graphs that plot a metric over time. They are fantastic for quickly spotting shifts, trends, or patterns. For instance, plotting the monthly infection rate after starting a new hand-hygiene campaign can show at a glance if the change is making a lasting difference.
Control charts are a souped-up version of a run chart. They add statistically calculated upper and lower control limits, which help you tell the difference between "common cause variation" (the normal, everyday static in a process) and "special cause variation" (a significant change that signals a real shift in performance). This is crucial—it stops your team from overreacting to minor dips and spikes while flagging the big changes that demand investigation.
Investing in these kinds of measurement systems is becoming the norm. The global market for healthcare quality management is expected to jump from USD 4.4 billion in 2025 to USD 12.7 billion by 2034. That massive growth underscores just how much the industry is banking on data to drive safer, more effective care.
By combining the right metrics with clear visual tools, you give your team the power to use data not just for reports, but as a live tool for learning, adapting, and making real, sustainable improvements for your patients.
Overcoming Common Implementation Challenges

Starting a quality improvement project in healthcare is a lot like trying to change the course of a massive ship. You can have the perfect navigation chart, but you’re still going to hit rough waters. Even the most well-designed initiatives run into real-world obstacles that can stall them out.
Getting through these hurdles takes more than just a good plan. It requires a genuine understanding of the human, financial, and technical roadblocks that will inevitably pop up. Knowing what’s coming is the first step to building a project that can actually deliver lasting improvements for both patients and staff.
The Human Element: Resistance to Change
Often, the biggest barrier isn't a broken process or a lack of data—it's people. Healthcare professionals are under immense pressure, and they can be understandably skeptical of new workflows, especially if past initiatives have fizzled out. The phrase "this is how we've always done it" is a powerful force for a reason.
This resistance usually comes from a place of fear or feeling overlooked. That’s why communication is so critical. Leaders have to sell the "why" behind the change, making a direct line from the project to better patient outcomes and a less frustrating workday for the team.
Creating a culture of psychological safety is absolutely essential. This means fostering an environment where staff can voice concerns, point out problems, and suggest ideas without worrying about blame. When people feel safe and heard, they stop being roadblocks and start becoming part of the solution.
Building trust is the bedrock of any successful quality improvement project. When teams feel safe and valued, they are far more willing to try new things, adapt on the fly, and take collective ownership of the results.
Navigating Resource Constraints
Let's be realistic: another common roadblock is the lack of resources. Most healthcare organizations run on tight budgets and lean staffing. This makes it tough to carve out the time and money needed for significant healthcare quality improvement initiatives. The very idea of a huge project can feel completely overwhelming before it even gets off the ground.
The best way forward? Think small to win big. Don’t try to fix everything at once.
- Identify Quick Wins: Go after a process that is a known pain point for everyone and has a relatively simple fix.
- Demonstrate Value: When you successfully improve that one small but annoying thing, you provide tangible proof that this QI stuff actually works.
- Build Momentum: These early victories generate real enthusiasm and build the credibility you need to ask for more resources for bigger projects later on.
This step-by-step approach makes the whole effort feel manageable. It also delivers tangible results fast, which is crucial for keeping your team motivated and leadership invested.
Tackling Data and Technical Hurdles
Data is the fuel for any quality improvement engine, but getting it, managing it, and making sense of it can be a huge technical headache. Teams often wrestle with clunky electronic health record (EHR) systems, a lack of good analytical tools, or data that’s locked away in different departmental silos.
These issues have real consequences. Delays in getting the right information to the right person directly impact patient care. For instance, 33% of patients report that delayed specialist consultations made their health worse, and for more than a quarter, it even led to hospitalization. The 2025 Philips Future Health Index dives deeper into these kinds of challenges.
For teams that don't have a dedicated data analyst, the key is to keep it simple. If you have to, start by collecting data manually on a small scale. Use basic tools like spreadsheets to track what’s happening. Of course, when you’re dealing with patient information, security is non-negotiable. Sticking to a clear set of HIPAA compliance requirements is fundamental. By focusing on just the essential data and keeping it secure, even teams with limited tech can drive powerful change.
Real-World Examples of Successful Initiatives
Theory and frameworks are one thing, but the real magic of healthcare quality improvement initiatives happens on the ground. This is where you see how structured, data-driven thinking can lead to profound, life-saving results. These stories from the front lines offer a clear blueprint for turning persistent problems into lasting solutions.
Let's step away from the abstract and look at some concrete examples of organizations that have genuinely transformed patient care. Each case breaks down the problem, the strategy, the outcome, and the key lessons anyone in healthcare can take away.
Reducing Surgical Site Infections with Six Sigma
A large hospital system was grappling with a high rate of surgical site infections (SSIs) after certain major operations. These infections weren't just dangerous for patients—leading to longer stays and more readmissions—they were also incredibly costly for the hospital.
The Problem: The existing infection control protocols were all over the place. There was a huge amount of variation in how different surgical teams prepped patients, managed the operating room, and handled post-operative care.
The Strategy: The hospital decided to go all-in with the rigorous, data-focused Six Sigma methodology. They pulled together a cross-functional team of surgeons, nurses, and anesthesiologists to map out the entire surgical process from start to finish. Using the DMAIC (Define, Measure, Analyze, Improve, Control) framework, they pinpointed the exact moments where things were most likely to go wrong.
The Results: After digging into the data, the team rolled out a standardized "bundle" of evidence-based practices that became mandatory for every single surgery. This included specific pre-op skin cleaning protocols, precise antibiotic timing, and strict traffic control in the OR. The impact was stunning: within 18 months, the hospital slashed its SSI rate for these procedures by an incredible 70%.
The Lesson: Standardization is an incredibly powerful tool for getting rid of errors. By taking the guesswork and variability out of a critical process, the team made the safest path the easiest path for everyone to follow.
This initiative proves a core principle of quality improvement: You don't get better by just hoping for better outcomes. You get better by designing and implementing better processes that make positive outcomes almost inevitable.
Cutting Patient Wait Times Using Lean Principles
A network of busy primary care clinics was dealing with a familiar but maddening issue: long patient wait times. It was common for patients to sit in the waiting room for 30 to 45 minutes past their appointment time, which tanked satisfaction scores and stressed out the front-office staff.
The Problem: The appointment and check-in processes were riddled with "waste"—unnecessary steps and bottlenecks that caused delay after delay. The workflow was chaotic, with information being handled multiple times and patients moving haphazardly through the clinic.
The Strategy: The clinics adopted Lean principles to get their operations in order. They started with a "value stream map," a visual tool that diagrams every single step in a patient's journey, from booking the appointment to seeing the doctor. This immediately brought several points of friction into sharp focus.
They discovered, for instance, that 40% of check-in time was spent on paperwork that could have been done before the visit. They also realized the clinic's physical layout forced nurses to walk long distances for supplies, adding minutes to every single patient encounter.
The Results: Armed with these insights, the clinics completely redesigned their workflow. They launched an online portal for pre-visit paperwork, reorganized supply closets to be closer to exam rooms, and created a simple visual signal system so the team knew which rooms were ready. The payoff was huge: the average patient wait time dropped by over 50%, down to just 15 minutes.
The Lesson: A series of small, logical changes can add up to a massive effect. By focusing on eliminating wasted time and effort, the clinics not only made patients happier but also created a smoother, less stressful workday for their staff. This kind of transformation is a perfect example of how the principles behind workflow automation in healthcare can be applied to optimize manual processes, too.
Preventing Hospital Readmissions with Predictive Analytics
A major health system was getting hit with financial penalties because of high 30-day readmission rates for patients with chronic conditions like heart failure and COPD. They knew they needed a more proactive way to support these high-risk patients once they left the hospital.
The Strategy: The organization leaned into technology, implementing a predictive analytics platform. The system scoured data from electronic health records—including past admissions, lab results, and medications—to generate a "risk score" for every patient at the time of discharge.
The Results: Any patient flagged as high-risk was automatically enrolled in an intensive transitional care program. This meant a follow-up call from a nurse within 48 hours of discharge, home visits from a community paramedic, and automated medication reminders via text. This targeted approach led to a 25% reduction in readmissions for this high-risk group in the first year alone, saving millions and dramatically improving patient safety.
The Lesson: Using technology to see problems coming before they happen is a game-changer. By focusing their limited resources on the patients who needed them most, the health system delivered more effective, personalized care and prevented countless people from having to come back to the hospital.
The Future of Healthcare Quality Improvement
The world of healthcare quality isn’t static. It’s constantly being reshaped by new technology and, just as importantly, by a growing understanding of what quality actually means to patients. As we look ahead, the next wave of healthcare quality improvement initiatives will feel far more predictive, personalized, and patient-driven than anything we’ve seen before.
This isn’t some far-off, futuristic vision. Forward-thinking health systems are already putting these ideas into practice. From artificial intelligence that can anticipate a patient's needs to care models that reward better health outcomes, the entire field is shifting from being reactive to proactive.
The Rise of Predictive Analytics and AI
Artificial Intelligence (AI) and machine learning are quickly moving from the fringes to the center of quality improvement work. Instead of just analyzing what went wrong after the fact, these tools can dig through mountains of data—EHRs, real-time vitals, lab results—to spot risks before they snowball into crises.
Think about it: what if a system could flag a patient as having a high probability of developing sepsis hours before the classic symptoms even appear? That early warning gives clinical teams a crucial head start, letting them intervene and turn a potentially fatal condition into something manageable. This predictive power is popping up everywhere:
- Spotting High-Risk Patients: AI algorithms can pinpoint which patients are most likely to be readmitted, allowing hospitals to wrap extra support around them after discharge.
- Personalizing Treatment: By crunching genetic data, lifestyle factors, and outcomes from thousands of similar patients, AI can help a doctor choose the most effective path for the person right in front of them.
- Smoothing Out Hospital Operations: Machine learning can forecast patient flow, helping hospitals get ahead of staffing needs and bed shortages. The result? Shorter wait times and less chaos.
This kind of data-driven foresight is a game-changer. We're finally moving from looking in the rearview mirror to looking at the road ahead.
Extending Care Beyond Hospital Walls
High-quality care can no longer be something that only happens within a clinic or hospital. With the explosion of telehealth and remote patient monitoring (RPM), healthcare providers can now keep a supportive eye on patients long after they’ve gone home.
These technologies are proving essential for managing chronic diseases and helping people recover safely. For instance, a patient getting back on their feet after heart surgery can use RPM devices to send daily updates on their weight, blood pressure, and oxygen levels right to their care team.
This constant stream of data lets clinicians see when a trend is heading in the wrong direction and step in immediately. It can be the difference between a quick phone call and a trip back to the emergency room, transforming care from a series of disconnected appointments into a continuous partnership.
Telehealth also smashes through geographic barriers. A patient living in a rural community can now get direct access to a specialist hundreds of miles away. This is a huge win for the equity dimension of quality, making sure your zip code doesn’t dictate your health outcome.
A Deeper Focus on Patient-Reported Outcomes
For years, quality improvement was all about clinical metrics like infection rates or mortality. Those numbers are still vital, of course, but they don't paint the full picture. The future of healthcare quality is leaning heavily into Patient-Reported Outcomes (PROs).
PROs are exactly what they sound like: they’re direct reports from the patient on how they’re feeling and functioning. This simple shift in perspective puts the focus squarely on what matters most to the person receiving the care.
Here’s why this is so important:
- Measuring what matters: Asking someone with arthritis if their pain stops them from gardening tells you more about treatment success than a lab test ever could.
- Fueling shared decision-making: When doctors understand a patient’s personal goals, they can collaborate on a care plan that actually aligns with those priorities.
- Driving real-world improvement: By collecting PROs from thousands of patients, a health system can figure out which treatments deliver the biggest boost to quality of life and channel their improvement efforts there.
This focus ensures that healthcare quality improvement initiatives are tied to the ultimate goal: helping people live healthier, more fulfilling lives. It’s a patient-centric view that is fundamentally changing how we define success.
At Whisperit, we know that solid, accurate documentation is the bedrock of any serious quality improvement effort. Our AI-powered dictation platform helps healthcare professionals capture detailed patient notes up to two times faster, giving them back precious time to focus on what they do best—delivering exceptional care. Secure, compliant, and built for the real-world demands of modern healthcare, Whisperit helps you streamline your workflow so you can help drive the future of quality. Find out how to transform your documentation process at https://whisperit.ai.