Voice Recognition Medical Software Guide
Think of voice recognition medical software as your personal digital scribe, one that listens to your clinical notes and instantly turns them into structured text right inside a patient's electronic health record. It’s a game-changer that helps clinicians capture detailed patient encounters up to five times faster than typing it all out by hand.
The End of Administrative Overload
For too many doctors, the day doesn't wrap up when the last patient heads home. It often drags on for hours, buried under a mountain of administrative work and clinical documentation. This dreaded "pajama time" spent catching up on charts is a massive contributor to burnout, chipping away at time that should be spent on patient care or with family.
Now, what if you had an expert scribe with you for every single patient visit? One that never gets tired, flawlessly understands complex medical jargon, and types as fast as you can speak. That’s exactly what voice recognition medical software brings to the table. It’s far more than a simple dictation app; it's a smart system built to navigate the complex world of modern healthcare.
Beyond Basic Dictation
Unlike the voice-to-text feature on your phone, these specialized platforms are designed from the ground up with clinical workflows in mind.
- They speak your language. These tools are trained to accurately recognize and write out everything from complex drug names to specific surgical procedures with incredible precision.
- They structure notes for you. The software can automatically format your dictation into standard clinical notes, like the SOAP (Subjective, Objective, Assessment, and Plan) format, keeping everything consistent and easy to read.
- They integrate with your existing systems. It connects directly into your practice’s Electronic Health Record (EHR) or Electronic Medical Record (EMR) system. This means your spoken notes land in the right patient file without any clumsy copy-pasting.
This seamless integration turns documentation from a clunky, multi-step chore into a natural, conversational part of the patient visit.
This isn't just a fleeting trend. We're seeing a fundamental shift in how healthcare administration is handled. By taking on one of the biggest administrative headaches, this technology helps close the efficiency gap that bogs down so many medical practices.
The numbers back this up. The global market for this technology was valued at USD 1.73 billion in 2024 and is expected to soar to USD 5.58 billion by 2035. This boom is driven by the urgent need to make clinical work more efficient and ease the administrative strain on medical professionals.
We're already seeing this in action. For example, the integration of DAX Copilot with Epic's EHR at Northwestern Medicine shows how these tools can capture a patient conversation and turn it into clinical documentation in real-time. You can explore more about this market trend to see the full picture. It’s becoming clear that adopting voice recognition is a crucial move for any practice looking to win back precious time and refocus on what truly matters: patient outcomes.
How This Technology Actually Works

At its core, voice recognition medical software is less like a simple dictation machine and more like a highly specialized medical scribe. It’s not just hearing words and typing them out; it’s an intelligent system designed to understand the complex language of medicine, listen to clinical conversations, and document them accurately—all while staying completely in the background.
This isn’t magic, but a powerful combination of three key technologies working in concert: Artificial Intelligence (AI), Machine Learning (ML), and Natural Language Processing (NLP). You can think of AI as the system's brain, ML as its ability to learn from experience, and NLP as its deep understanding of human language. Together, they turn spoken dialogue into structured, clinically useful data.
The whole process kicks off with speech-to-text conversion. When a doctor speaks, the software captures the sound waves and breaks them down into their smallest audible parts, known as phonemes. The AI then references enormous language models to piece these sounds back together into words and sentences, effectively translating sound into digital text.
From Simple Dictation to Ambient Intelligence
But that’s just the first step. Where modern systems really shine is in their capacity to learn and adapt, which is where Machine Learning enters the picture. Much like a human scribe gets better by learning a specific doctor's habits and accent, the software's ML algorithms constantly fine-tune their performance over time.
This continuous learning helps the software:
- Adapt to Individual Accents: The system gets familiar with the unique cadence, pitch, and accent of a clinician's voice, making it more accurate with each use.
- Distinguish Between Speakers: In a busy exam room, it can tell the difference between the doctor, the patient, and a nurse, attributing each part of the conversation correctly.
- Interpret Medical Jargon: It comes pre-loaded with a massive dictionary of medical terms, drug names, and procedures, so it knows "metformin" isn't "met for men."
This evolution has given rise to one of the biggest leaps in clinical documentation: ambient listening. Instead of a doctor having to actively dictate into a device, ambient technology just listens to the natural, free-flowing conversation during a patient visit. It intelligently picks out the medically relevant details and drafts a clinical note automatically, without needing any specific commands.
The core goal of this technology is to make the computer disappear from the exam room. By handling documentation silently in the background, it allows clinicians to restore face-to-face interaction, build patient rapport, and focus entirely on providing care.
The Power of Understanding Language
The final piece of this technological puzzle is Natural Language Processing. NLP is what gives the software its "smarts"—the ability to understand context. It’s the engine that moves the system beyond simple transcription and into actual comprehension of medical conversations. For a deeper look into the specifics, our guide on medical voice recognition provides further details.
For instance, NLP is what allows the software to:
- Identify Key Clinical Concepts: It pulls out diagnoses, medications, symptoms, and treatment plans directly from the conversation.
- Structure the Narrative: It can organize that information into the proper sections of a standard clinical document, like a SOAP note.
- Recognize Intent: It understands the difference between a doctor asking a question ("Have you ever had chest pain?") and making a diagnosis ("The patient has chest pain.").
The real-world result of all this is a game-changer. It frees clinicians from the tyranny of the keyboard, letting them look their patients in the eye again. This doesn't just cut down on documentation time; it brings the human element back to the forefront of the consultation, ultimately leading to better care.
Key Features That Drive Clinical Efficiency
Not all voice recognition medical software is created equal. When you move past the core technology, you'll find that certain features are what really separate a powerful clinical tool from a basic dictation app. These are the elements that don't just turn speech into text; they actively speed up workflows, cut down on administrative headaches, and give clinicians back their most valuable asset: time.
For any practice leader or physician trying to make a smart investment, understanding these features is non-negotiable. Let’s break down what truly matters.
Flawless Medical Vocabulary And Accuracy
The absolute bedrock of any good medical voice recognition tool is its ability to understand the unique language of healthcare. Your standard consumer-grade dictation app will stumble over complex medical terms, forcing you into a frustrating cycle of corrections. Clinical-grade software is built differently from the ground up.
It comes packed with a massive, specialty-specific vocabulary that covers everything from pharmacology to intricate surgical procedures. This means when a doctor says "amoxicillin" or "laparoscopic cholecystectomy," the software gets it right the first time. The best platforms out there boast accuracy rates hitting 99% and get even smarter over time by learning a specific user’s accent and speech patterns.
This image really drives home the difference in speed and time saved when you compare manual typing to using specialized voice recognition.
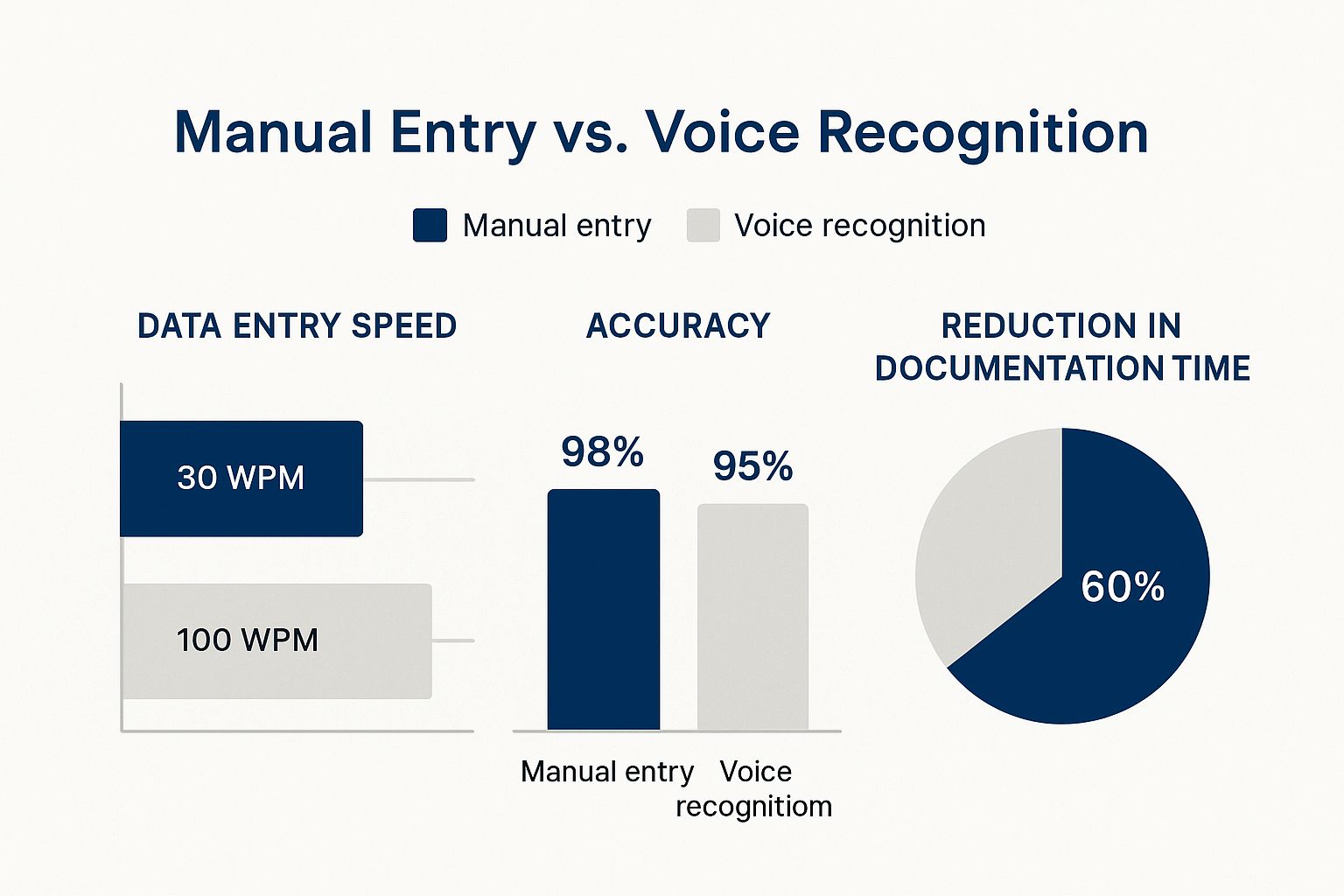
It’s clear that while manual typing might seem a tiny bit more accurate, the incredible gains in speed completely change the productivity equation for a busy day.
Seamless EHR And EMR Integration
A dictation tool that exists in a vacuum is more trouble than it's worth. If your team is constantly copying and pasting text, you haven't solved the problem. Real efficiency is born from deep, seamless integration with the Electronic Health Record (EHR) and Electronic Medical Record (EMR) systems you already use.
This feature allows a clinician to dictate straight into the right fields within a patient’s chart. Think about it: you dictate a patient's story, and it instantly populates the "History of Present Illness" section. No clumsy workarounds, no manual data entry. This keeps the data clean and puts it exactly where it needs to be.
For any serious clinical setting, this level of integration isn't just a nice-to-have; it's a must-have. It turns the software from a simple add-on into a core part of your practice’s workflow, making documentation feel completely natural.
The goal is to make documentation an invisible, background task. Seamless EHR integration means the clinician can focus on the patient's narrative, knowing their words are being captured and correctly filed without a single extra click.
Customizable Templates And Voice Commands
Here’s where the real magic happens. One of the most powerful efficiency drivers is the ability to create custom templates and voice-activated macros. So much of clinical documentation is repetitive, following a standard format for common visits.
Instead of saying the same phrases over and over, a clinician can create a simple voice command. For example, saying "insert normal physical exam" could instantly drop a full, detailed paragraph into the note. A task that used to take five minutes of typing is now done in five seconds.
But it goes way beyond just text snippets. Clinicians can build custom commands to do almost anything:
- Navigate the EHR: Use your voice to open a patient's chart, jump to the lab results, or sign off on a note.
- Order Prescriptions: Dictate a command like "prescribe metformin 500mg" to pull up the prescription module automatically.
- Insert Standardized Text: Create shortcuts for patient instructions, referral letters, or common assessment and plan notes.
These personalized shortcuts slash the number of clicks and keystrokes needed every day, and those saved seconds add up to hours over the course of a week.
The global market for medical transcription software, which is the engine behind these systems, was valued at USD 2.55 billion in 2024 and is expected to soar to USD 8.41 billion by 2032. This explosive growth is a direct result of demand for these kinds of efficiency-boosting features as the healthcare industry looks for ways to combat physician burnout. You can discover more insights on the market's trajectory at Fortune Business Insights.
Mobile Accessibility For On-The-Go Dictation
Clinical work doesn't stop at the desktop. Doctors and nurses need to document while doing rounds, walking between patient rooms, or even catching up from home after hours. Quality voice recognition medical software provides solid mobile apps that sync perfectly with the main desktop platform. You can learn more about how this works in our guide on AI-powered voice-to-text technology.
This kind of flexibility is a game-changer. A clinician can start a note on their phone while walking down the hall and then seamlessly finish it at their desk without losing a single word. It allows documentation to happen in the moment, preventing a mountain of notes from piling up at the end of a long and demanding day.
Comparison of Key Software Features
To make sense of the options, it helps to see how features stack up across different types of software. From simple dictation tools to fully integrated platforms, the capabilities can vary significantly.
| Feature | Basic Software | Advanced Platform | Importance in Clinical Workflow |
|---|---|---|---|
| Medical Vocabulary | General or limited specialty | Extensive, specialty-specific, and self-learning | Critical: Prevents constant, time-wasting corrections. |
| EHR/EMR Integration | None; requires copy-paste | Deep, direct integration into chart fields | Essential: Eliminates manual data entry and ensures accuracy. |
| Custom Templates | Basic text replacement | Voice-activated macros for complex notes and actions | High: Dramatically speeds up repetitive documentation tasks. |
| Voice Commands | Limited to "start/stop" dictation | Navigates EHR, places orders, signs notes | High: Reduces clicks and streamlines the entire workflow. |
| Mobile Access | Often none or a separate, non-synced app | Fully synced mobile app for on-the-go dictation | Medium to High: Provides crucial flexibility for busy clinicians. |
| Ambient Intelligence | Not available | Captures conversation and auto-drafts notes | Transformative: Moves documentation into the background. |
Ultimately, the right choice depends on your practice's needs, but this comparison highlights why advanced platforms with deep integration and customization are so impactful in a real-world clinical environment.
Real-World Benefits for Doctors and Patients
Forget the technical jargon for a moment. The real impact of voice recognition medical software isn’t measured in processing speed, but in real human outcomes. We're talking about a fundamental shift in the day-to-day grind for clinicians and a massive upgrade in the quality of care patients receive. This isn't just about writing notes faster; it's about reshaping the entire clinical encounter for the better.
Think about a primary care physician's typical day. Without this software, every patient visit becomes a race against time, a frantic split between listening to the patient and typing into a computer. The doctor's focus is divided, their eyes flicking back and forth from the person in front of them to the screen. The result? Incomplete notes, a weak patient connection, and the dreaded "pajama time"—those extra hours spent at home finishing charts that lead straight to burnout.
Now, let's replay that same day with modern voice recognition. The physician walks into the exam room and gives the patient their complete, undivided attention. As they talk, an ambient system works quietly in the background, capturing the conversation and intelligently drafting a clinical note. Eye contact is steady, trust is built, and the focus stays exactly where it should be: on the patient. The doctor actually leaves work on time, their documentation is done, and they feel more like a healer and less like a data entry clerk.
A New Standard for the Patient Experience
This change completely transforms the experience from the patient's perspective. When the doctor isn't shackled to a keyboard, the entire dynamic in the exam room improves.
- Better Communication: Patients feel genuinely heard when their doctor is looking at them, not a screen. This encourages them to open up and share important details about their health they might have otherwise held back.
- Higher Patient Satisfaction: The simple act of maintaining eye contact builds an incredible amount of rapport and trust. Patients walk away from their appointments feeling like they were seen and understood, which is the bedrock of great care.
- Improved Health Outcomes: When communication is crystal clear, patients are far more likely to stick to their treatment plans. They understand their diagnosis and what comes next, which directly leads to better results.
By getting the computer screen out of the way, the software puts the human connection back at the heart of medicine.
Studies have shown that physicians can spend up to two hours on administrative tasks for every one hour of direct patient care. Voice recognition software directly attacks this imbalance, reclaiming critical time for what matters most.
The Financial and Operational Upside
The positive effects don't stop in the exam room; they ripple out across the entire healthcare organization. There’s a reason the market for this technology is booming, projected to jump from USD 2.1 billion in 2024 to USD 12.5 billion by 2037. This explosive growth is driven by real-world results, especially as the need for efficient EHR documentation becomes non-negotiable. You can read the full research on the healthcare voice technology market for a deeper dive into these trends.
For hospital administrators and practice managers, the business case is crystal clear. Investing in voice recognition medical software delivers on multiple fronts:
- Reduced Clinician Burnout: When you eliminate hours of after-hours charting, you directly improve a physician's work-life balance. This boosts morale and cuts down on the high cost of staff turnover.
- Increased Throughput: Slashing documentation time in half means clinicians can either see more patients or spend more quality time on complex cases, both of which improve practice revenue and overall efficiency.
- Enhanced Billing Accuracy: More detailed, accurate clinical notes lead to more precise medical coding. This means fewer claim denials and ensures the practice is properly reimbursed for the care it provides.
At the end of the day, this isn't just another piece of software. It’s a strategic investment in the quality of your care, the efficiency of your operations, and the well-being of both your doctors and their patients. If you're looking for more ways to streamline your processes, check out our guide to improve clinical documentation.
Protecting Patient Data with Secure Technology

The efficiency gains from voice recognition are impressive, but they’re meaningless if patient privacy isn't ironclad. In healthcare, protecting sensitive information isn't just a good idea—it's a legal and ethical imperative.
Whenever you bring new technology into a clinical setting, especially one that processes Protected Health Information (PHI), you have to ask the tough questions about compliance and security. The best software providers get this. They've built their platforms from the ground up with multiple layers of security designed to meet and even exceed strict regulations like HIPAA.
The Role of End-to-End Encryption
At its core, powerful security begins with end-to-end encryption. Think of it as a digital sealed envelope. From the instant a clinician speaks into the microphone until the moment that audio is transcribed and stored, the data is completely scrambled.
This makes the information unreadable to anyone who might try to intercept it. It’s a non-negotiable feature for protecting data both in transit over the internet and at rest on a server.
Secure Cloud Environments And HITRUST
Where patient data lives is just as important as how it gets there. This is why leading medical voice recognition platforms use highly secure cloud infrastructure. But not just any cloud service will do; the real gold standard is a HITRUST-certified data center.
HITRUST certification is a demanding security framework that goes beyond basic HIPAA requirements. When you're looking at your options, consider solutions like cloud hosting specifically for healthcare applications that are purpose-built for the job.
A vendor's commitment to security speaks volumes. Choosing a platform hosted in a secure, compliant environment is one of the most critical decisions you can make.
On top of a secure environment, access controls are vital. Features like multi-factor authentication (MFA) add another crucial line of defense, requiring more than just a password to get in. This makes it significantly harder for the wrong people to access sensitive clinical notes.
The Critical Importance of a Business Associate Agreement
Finally, let's talk about one of the most important documents in this whole equation: the Business Associate Agreement (BAA). Under HIPAA, any third-party vendor that handles PHI for you is legally considered a "Business Associate."
A BAA is a formal contract that binds the software vendor to:
- Properly safeguard all the PHI they come into contact with.
- Adhere to all applicable HIPAA rules.
- Immediately report any data breaches.
Without a signed BAA, your organization is simply not HIPAA compliant. Period. It's an absolute must-have. When a vendor readily provides a BAA, it signals they understand their responsibilities and are serious about data protection. For a deeper dive, check out our guide on https://www.whisperit.ai/blog/hipaa-compliant-speech-to-text. This is the kind of assurance administrators need to adopt new tools with complete confidence.
Your Roadmap for Successful Implementation
Bringing new voice recognition software into your practice isn't like flipping a switch. It’s a deliberate process, one that needs a solid plan to get your team on board and see real results. If you break it down into manageable steps, you can navigate the change smoothly and unlock the software's full potential from day one.
The journey starts by taking a hard look at your current workflow. Before you even think about talking to vendors, you need to understand your practice's biggest documentation headaches. Are your clinicians spending too much time on EHR notes after hours? Is repetitive data entry causing burnout? Are records inconsistent from one provider to the next? Nailing down these pain points gives you a "must-have" feature list to guide your search for the right solution.
With that checklist in hand, you can start evaluating vendors. Look for a partner who not only has the right features but also genuinely understands the realities of a healthcare setting and has rock-solid security protocols.
Planning a Pilot Program
Instead of rolling out the new software to everyone at once, I always recommend starting small with a pilot program. This lets you test the voice recognition medical software in a controlled setting, maybe with a single department or a handful of tech-savvy clinicians who are excited to try it.
A pilot program is incredibly useful for a few reasons:
- Demonstrates Value: It creates a clear, in-house case study showing exactly how the software improves efficiency and makes clinicians' lives easier.
- Gathers Feedback: You'll get honest, real-world feedback from users, which you can use to tweak settings and workflows before the full launch.
- Builds Momentum: A successful pilot creates "champions" for the new tool—respected colleagues who can share their positive experiences and help train their peers.
This phased approach takes the pressure off. It turns what could be a disruptive, stressful change into a collaborative and much more manageable project.
Driving Adoption Through Training and Support
Let's be honest: the biggest hurdle is almost always getting people to embrace a new way of doing things. The secret is making the transition feel as seamless as possible with great training and continuous support. Find your "physician champions"—those respected clinicians who are genuinely enthusiastic about the tech—and get them to lead the charge. Their buy-in is often more powerful than any top-down mandate.
Your training shouldn't be a one-and-done deal. Plan for regular check-ins and offer more advanced sessions down the road to help your team master cool features, like building their own voice commands or custom templates.
Good training turns hesitation into confidence. For clinicians wanting to dive deeper into optimizing their charting, our guide on documentation workflow management offers strategies that pair perfectly with this technology. When you match the right tool with a thoughtful implementation plan, you give your team the freedom to focus on what actually matters: their patients.
Common Questions About This Technology

It’s completely normal to have a few practical questions before bringing a new tool into your practice. You need to know how it will really perform, how it affects your team, and what it takes to get up and running. So, let’s get straight to the answers for the most common questions we hear.
How Accurate Is Modern Medical Voice Recognition?
If you tried voice recognition years ago, you might be skeptical. But today's systems are a world apart from those clunky, error-prone tools. Thanks to huge leaps in AI, the best platforms now consistently achieve 99% accuracy or better, putting them on par with highly skilled human transcriptionists.
How do they get it so right? The software is built to learn. It quickly adapts to a specific doctor's accent, speaking rhythm, and even their unique phrasing. Plus, these systems come pre-loaded with extensive medical vocabularies, so they understand complex terminology right out of the box.
The real game-changer is the software’s ability to grasp context. It doesn't just hear words; it recognizes medical jargon, drug names, and procedures, which drastically cuts down on the need for manual edits.
This level of precision is what makes the technology so reliable. Clinicians can speak naturally, trusting that the software will capture a clean, professional record of the patient visit. It stops being a neat gadget and becomes an indispensable part of the clinical toolkit.
Will This Software Replace Our Scribes or Transcriptionists?
This is probably the biggest concern we hear, but the goal of this technology isn't replacement—it's elevation. Think of it as a powerful assistant that handles the most tedious part of documentation: getting that first draft down.
By automating the initial transcription, you free up your scribes and transcriptionists to work on tasks that truly require a human touch. Their roles often evolve to focus on:
- Quality Assurance: Reviewing and polishing AI-generated notes, especially for complex cases where nuance is critical.
- Workflow Management: Overseeing the documentation process to make sure every note is finalized, accurate, and filed on time.
- Specialized Editing: Handling particularly sensitive patient records that benefit from careful human judgment.
In the end, the software makes these team members more efficient and more valuable. They can manage a higher volume of work with an even greater focus on quality control.
What Kind of Training Is Required for Our Clinicians?
You'll be pleasantly surprised by how quickly your team can get started. The best platforms are designed to be intuitive, with interfaces that feel familiar to anyone who uses a smartphone or computer daily. For basic dictation, most clinicians are comfortable and working efficiently within a couple of hours.
Of course, mastering the more advanced features—like building custom templates or creating voice commands to navigate the EHR—takes a little more practice. But with good onboarding from the provider, most users can get the hang of these powerful shortcuts in just a few days, unlocking even bigger time savings in their daily routines.
Ready to cut your documentation time in half and refocus on patient care? Whisperit provides a secure, AI-powered dictation platform designed for the demands of modern healthcare professionals. Learn how Whisperit can transform your clinical workflow.